Head & Neck Cancer and Human Papillomavirus (HPV)

What is Head and Neck Cancer?
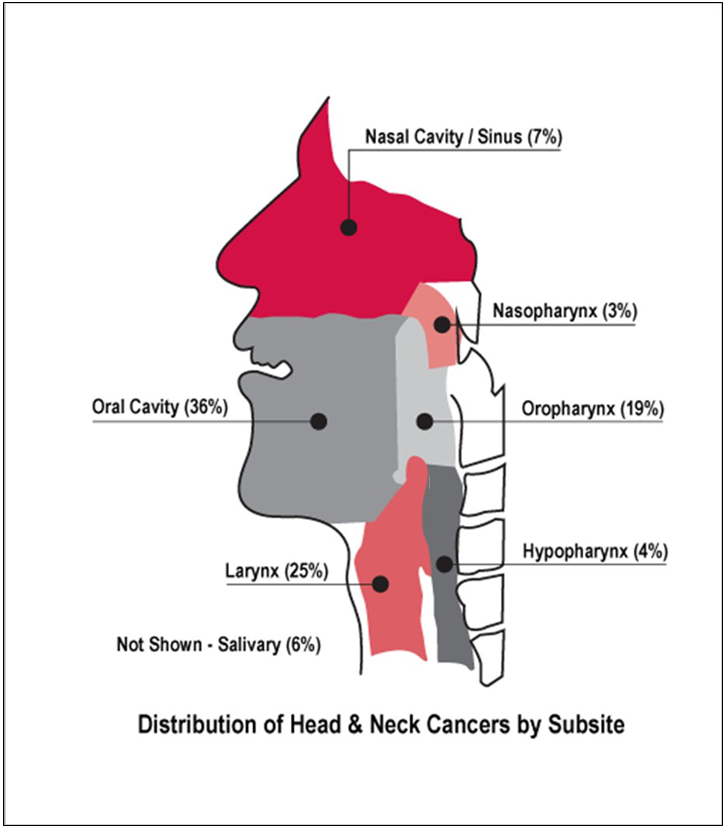
Cancers that start in the head, mouth, nose, tongue and throat are called head and neck cancer. All cancers are named after the area of the body where the cancer starts. Some of the areas of the head and neck where cancer can start are highlighted in the diagram to the right. Cancer happens when cells in the body start to grow out of control. Cancer can happen in nearly all cells of the body and can spread to other parts of the body.
Head and Neck Cancer Information
Facts about Head and Neck Cancer
About 3% of all cancers in the United States are head and neck cancers. Men are twice as likely to get head and neck cancers as women are. More of the cancers are in people over age of 40; however, the number of younger people with head and neck cancers is going up. Oropharyngeal cancer (back of the mouth and throat) caused by HPV infection without other risk factors like tobacco use or drinking has increased dramatically over the last 20 years in young men and women. The American Cancer Society estimates that there could be more than 85,000 cases of head and neck cancers in 2021.
(Graphic from Head & Neck Cancer Alliance (www.headandneck.org))
What are the types of Head and Neck Cancer?
There are many types of head and neck cancers.
Here is a list of the common types:
- Oral cavity cancer – starts in the mouth
- Oropharyngeal cancer – starts in the back of the mouth or throat
- Nasal cavity cancer – starts in the opening behind the nose, a space that runs along the top of the roof of the mouth and then turns downward to join the back of the mouth and throat
- Paranasal sinus cancer – starts in the openings called sinuses that are around or near the nose
- Nasopharyngeal cancer – starts behind the nose in the upper part of the throat
- Laryngeal cancer – starts in the voice box or larynx
- Hypopharyngeal cancer – starts behind the voice box in the lower part of the throat
(List is from https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/if-you-have-head-or-neck-cancer.html)
What are the risk factors for Head and Neck Cancer?
- Tobacco – all forms; cigarettes, snuff, pipes, chewing tobacco, snus, cigars, and all vapor products. Tobacco use increases the risk of head and neck cancer by 15 times than people who do not use tobacco.
- Alcohol – heavy use increases the chances of developing cancer.
- Tobacco and Alcohol – use of tobacco and alcohol creates a greater risk of developing cancers than in people who use either alcohol or tobacco alone.
- Human Papillomavirus (HPV) – infection can develop into cancer.
- Oral Sex – with one to five partners over lifetime doubles the risk of HPV infection and cancer. The risk increases five-fold with six or more oral sex partners compared to people who have not had oral sex. Even people who have had sex with only one person in their lifetime can get HPV.
- Gender – men are more likely to get oral cancer.
- Age - oral cancer appears more in people over the age of 40 but has appeared in younger people and children.
- Sun Exposure – cancer in the lip can be caused by sun exposure.
- Diet – low consumption of fruits and vegetables may play a role in oral cancer.
- Oral Health – poor oral health and missing teeth may promote the development of oral cancer.
Many types of head and neck cancers are caused by HPV, but not all individuals who have HPV will develop cancer. This is where HPV screening can help you understand your risk. Some types of HPV are more likely to cause head and neck cancer, so testing to see if you have one of these high-risk types of HPV will help you understand your risk of developing HPV-related head and neck cancer.
What are the symptoms of Head and Neck Cancer?
The American Dental Association (ADA), National Cancer Institute (NCI) at the National Institutes of Health (NIH), CDC, American Cancer Society (ACS) plus other agencies/organizations recommend you see your dentist or doctor if the following signs or symptoms in the mouth, throat or lip do not go away after two weeks.
- A sore, lump, irritation, rough spot, crust, or thick patch that does not go away
- Red or white patches on gums, tongue or inside the cheek
- Pain, tenderness or numbness in mouth, tongue, other areas of the mouth or lips
- Difficulty chewing, swallowing or speaking
- Change in voice or hoarseness
- Swelling of the jaw that changes the way teeth fit together
- Unusual bleeding in mouth, nose or throat
- Pain in neck or throat, headaches or ringing in ears
- Blocked sinuses that do not clear or chronic sinus infections that do not clear when treated with antibiotics
- Trouble or swelling with eyes
- Swelling around the jaw and under the chin
Since symptoms usually are not evident until later, less treatable stages, this is why regular screening is so important!
Head and Neck Cancer Prevention
What can I do to prevent Head and Neck Cancer?
Get the Vaccine for HPV
- For maximum protection against HPV, vaccinate girls and boys between ages 9 to 12 with 2 doses of the vaccine.
- If you are 26 years or younger consult your dentist or doctor about the vaccines for HPV. People ages 27 to 45 may also receive the HPV vaccines if considered to be at high risk for HPV infections.
Screen Regularly
Guide to Monthly Self-Exams for Everyone
- Feel your neck for lumps.
- Using a mirror, look at the inside and outside of your lips and the inside of the cheeks.
- Bite gently and look at your gums.
- Using a flashlight and mirror, open your mouth and look at all sides (top, bottom, sides) of the tongue, back of the throat, the roof of the mouth and under the tongue.
How can my dentist help detect Head and Neck Cancer Early?
- During regular exams, the dentist will ask about changes in your health and if you have had any new or unusual symptoms.
- When your dentist checks your oral cavity, the will examine your lips, gums, tongue, inside of the cheeks, and floor and roof of your mouth. The dentist will also check your throat, tonsils and soft part of the roof of your mouth. The dentist will feel your jaw and neck for lumps or anything not normal. If the dentist does not perform an oral, head and neck exam, ask him or her to do the exam.
Where to find a Dentist
Need help finding a dentist?
Be Aware of Risk Factors
- Be aware of your risk factors. Men are more likely to get head and neck cancer as they get older.
- If you have a poor diet, eating more fruit and vegetables may decrease chances of developing cancer.
- Stop using tobacco products and reduce or eliminate alcohol consumption to reduce the risk of cancer in the oral cavity and larynx. Studies have shown that people who stop smoking cigarettes lower their risk of head and neck cancers in half (50%) within 5 to 9 years. Twenty years after people have stopped smoking lowers the risk to the same as for people who have never smoked. Studies have also shown that stopping alcohol use will decrease the risk of head and neck cancers.
- Condoms used correctly and a new one used every time during sex can provide some protection. Condoms do not cover every possible HPV-infected area of the body. Condoms should be put on before any contact and kept on until sex is finished.
- Limit the number of sex partners and avoid sex with people who have had many other partners.
Head and Neck Cancer Treatment
What happens if my dentist finds something suspicious?
Do not panic! The dentist will not be able to tell if what he or she is seeing is cancer or not. The dentist might ask you to return in a week or two to check you again to see if the area has healed. Your dentist may refer you for testing the day of your checkup or after the second checkup.
Diagnosis of Head and Neck Cancer
Head and neck cancers can be discovered through many different ways. A dentist or doctor may find possible cancers during a routine exam of the head, neck and mouth. Most often cancers are found after a person seeks treatment of a problem or symptoms.
Always share your medical history and any risks you have like tobacco or regular alcohol use. If the dentist or doctor thinks that the problem or symptom needs further evaluation you will be referred to an ear, nose and throat specialist (ENT) called an otolaryngologist or a head and neck surgeon.
The ENT will do a thorough exam. A pharyngoscopy may be used to see some parts of your throat. This can be done in the doctor’s office and is painless. Long-handled mirrors may also be used to see the deeper parts of the throat, the base of your tongue and part of the voice box. A tiny flexible fiber-optic scope may be passed through your nose to see areas of your head that cannot be seen by eyes or mirrors.
If additional tests are needed, any of the following may be used:
-
PanendoscopyPanendoscopy - this test will be done under general anesthesia. Scopes will be used to look more thoroughly at the throat, voice box, esophagus (tube to the stomach, trachea (windpipe) and the bronchi (airways off the windpipe in the lungs).
-
BiopsyBiopsy - A small sample of tissue is removed from the problem area. The tissue is examined in a lab to determine if the sample has normal cells or cancer cells and the type of cancer. Several biopsies may be taken.
-
Exfoliative cytologyExfoliative cytology - the doctor collects cells from the problem area by scraping it with a small tool. The cells are examined under a microscope.
-
Incisional biopsyIncisional biopsy - a piece of the tissue is cut from the problem area. Depending on the location of the problem area, this may be done in the doctor’s office after the area has been numbed or in the operating room under general anesthesia.
-
Fine needle aspiration (FNA)Fine needle aspiration (FNA) - the doctor uses a thin, hollow needle and syringe to remove cells from the problem area. The cells will be examined using a microscope. This type of biopsy is used mostly for lumps in the neck or in the lymph nodes.
-
HPV TestingHPV Testing - tissues from a biopsy that are squamous cell carcinoma (cancer), especially cells from the tonsil or base of the tongue are tested for the HPV DNA marker called p16. This marker is related to an HPV infection. HPV cancers seem to respond better to treatment than other cancers of the head and neck.
-
Blood TestsBlood Tests - blood tests can tell the doctor more about your overall health.
-
Imaging TestsImaging Tests - imaging tests may be ordered at different times during diagnosis and treatment to look at the problem area, to see if cancer has spread, to see if treatment is working, and to look to see if the cancer has returned after treatment. There are different types of imaging to use and include:
-
Chest x-raysChest x-rays - to see if cancer has spread to the lungs.
-
CT ScanCT Scan - provides a detailed view of the organs and soft tissue so your doctor can see the location of any tumors, if the tumor is growing into other tissue or if the cancer has spread to lymph nodes, lungs or other organs. CT Scans also provide a detailed look at facial bones to see if the bones are affected by cancer.
-
MRIMRI - – images are useful to examine the neck, brain and the surrounding soft tissues of muscle, fat or long nerves.
-
PET ScanPET Scan - PET scans are used when cancer has been diagnosed to see if the cancer has spread to the lymph nodes or other areas of the body especially if the doctor suspects the cancer may have spread but is not sure where. Sugar that contains a low level of radiation is injected into your blood during the PET scan. Cancer cells absorb more of this sugar than normal cells and are easier to see in the images.
Questions to Ask Your Dentist Regarding Cancer
What is my main problem?
Why do you think what I have is cancer?
Is there a chance I do not have cancer?
Would you please write down the kind of cancer you think I might have?
What do I need to do?
What will happen next?
What tests will I need to have?
Where will the test be done?
Who can explain the tests to me?
How and when will I get the results?
Who will explain the results to me?
What do I need to do next?
Why is it important for me to do this?
What happens after treatment?
You will see your cancer doctor for years after your treatment ends. It is important that you go to all of the appointments. The exams and test can help find new cancer or returning cancer sooner, helping you get treatments sooner to stop the cancer.
Resources to Support Head and Neck Cancer Survivors
A Survivorship Care Plan helps cancer patients that have completed treatment understand how to manage problems that can happen after treatment. Guidelines provide help on how to talk to dentists, doctors and other healthcare providers about follow-up care. Guidelines also have information on how to manage treatment effects.
- Head and Neck Cancer Alliance
- American Cancer Society’s Head and Neck Cancer Survivorship Care Guidelines
- Cancer.Net
- OncoLink
- Cancer Survivors
How can you reduce the risk of developing a second new cancer?
You are at a higher risk to develop a new cancer possibly in your head, neck, esophagus or lungs if you have been treated for head and neck cancers. A second new cancer is higher in people who use tobacco and drink alcohol. Stop tobacco use, stop or limit alcohol drinking, eat a healthy diet with plenty of vegetables and fruit, lose weight and stay physically active.
Learn more about stopping tobacco use:
- National Cancer Institute (NCI) or 800-4-CANCER (800-422-6237)
- Smokefree provides tools and tips and special pages for Veterans, women, teens, individuals 60+ and for Spanish speakers
- BeTobaccoFree.gov
- Tips From Former Smokers
- 800-QUIT-NOW (800-784-8669), 855-DÉJELO-YA (855-335-3569), Mandarin and Cantonese 800-838-8917, Korean 800-556-5564, Vietnamese 800-778-8440
- The Real Cost of Tobacco
- American Cancer Society
- Mayo Clinic
Head and Neck Cancer Rates and Deaths
Head and Neck Cancer Rates and Deaths in Missouri
According to the American Cancer Society, about 85,890 people will get head and neck cancers in 2021. About 30,150 people will die from head and neck cancers in 2021. Estimated New Cases and Deaths of Most Common Head and Neck Cancers in US, 2021
In 2017, in the US, 46,157 new cases of head and neck cancers were reported and 10,126 people died from these cancers. In Missouri, in 2017 there were 1,030 new cases of head and neck cancers and 211 people died from these cancers.
In Missouri, in 2017, men had 772 (70%) of the head and neck cancers cases. Women had 248 (30%) of the head and neck cancers in Missouri during 2017.
New Head and Neck Cancer Cases per 100,000 People in Missouri by Race and Gender, 2017
New Head and Neck Cancer Cases per 100,000 People in U.S. by Race/Ethnicity and Gender, 2017
The number of head and neck cancer cases in 2017 was about 13 per 100,000 for Missourians, which was slightly higher than the national rate of about 12. When rates were compared over several years, no major changes were found.
Annual Rates of New Head and Neck Cancers per 100,000 People in Missouri, 1999-2017
Annual Rates of New Head and Neck Cancers per 100,000 People in U.S., 1999-2017
New Head and Neck Cancer Cases in Missouri, All Ages, All Races/Ethnicities, Male and Female, 2013-2017 (Map)
Deaths from head and neck cancers in 2017 was 3 per 100,000 people in Missouri and in the US. More men in Missouri and in the US died from head and neck cancer. More White and Black men died from head neck cancers than men of other races and ethnicities did.
Head and Neck Cancer Deaths per 100,000 People in U.S. Compared to Missouri, 2017
Head and Neck Cancer Deaths per 100,000 People in U.S. by Race/Ethnicity and Gender, 2017
Map - Head and Neck Cancer Deaths in Missouri, All Ages, All Races/Ethnicities, Male and Female, 2013-2017 (Map)
Head and Neck Cancer Educational Resources
Head and Neck Cancer Educational Resources
- American Cancer Society (ACS)
- If You Have Head or Neck Cancer
- HPV and Cancer
- Oral Cavity and Oropharyngeal Cancer
- Nasal Cavity and Paranasal Sinus Cancer
- Nasopharyngeal Cancer
- Laryngeal and Hypopharyngeal Cancer
- American Dental Association (ADA) MouthHealthy.org
- Oral Cancer
- Top 5 Risk Factors for Oral Cancer
- Cancer and Dental Health
- HPV: Head, Neck and Oral Cancer
- HPV Vaccine and Oral Health
- Detecting Oral Cancer
- Centers for Disease Control and Prevention (CDC)
- Gut, British Medical Journal, Periodontal Disease, tooth loss, and risk of oesophageal and gastric adenocarcinoma: a prospective study,
- Head & Neck Cancer Alliance (HNCA)
- HPV Awareness and Education – HPVANDME, A Non-Profit Organization
- HPV Cancer Resources
- The Oral Cancer Foundation
- National Cancer Institute (NCI) at the National Institutes of Health (NIH)
- Oral Cavity, Pharyngeal and Laryngeal Cancer Prevention
- Oral Cavity, Pharyngeal and Laryngeal Cancer Screening
- HPV Vaccination Linked to Decreased Oral HPV Infections
- Cigarette Smoking: Health Risks and How to Quit
- Oropharyngeal Cancer Treatment (Adult)
- Childhood Oral Cavity Cancer Treatment
- Support for People with Oral and Head and Neck Cancer (SPOHNC) pronounced “Spunk” Local Chapter in St. Louis that meets in the David C. Pratt Cancer Center at Mercy Hospital St. Louis
- U.S. Public Health Service Chief Dental Officer Newsletter#51: August 18, 2020. See page 10 Periodontal Disease linked to Cancer (attach pdf)
HPV Information
What is Human Papillomavirus (HPV)?
Human Papillomavirus (HPV) is a group of more than 150 related viruses and each virus is given a number. Viruses are very small organisms, so small that a special microscope is needed to see them. The most common types of HPV are found on human skin and cause warts on hands, feet, arms and chest. Other types of warts are found on the body’s moist surface layers that line organs and parts of the body that open to the outside like the mouth, throat, vagina, anus and eyelids.
More than 40 of the 150 viruses are spread easily through direct skin-to-skin and during oral, vaginal and anal sex. Low-risk HPVs can cause all types of warts but the high-risk types can cause cancers. Most people who get an HPV infection will clear the infection. Their immune system will attack the virus and clear the infection within 2 years. Sometimes, the infection does not go away. A long lasting or chronic infection especially the high-risk HPV types can cause cancer over time.
Due to the many types of HPV, you may get several different types during your life. You can have the same type more than once but the chance of this is low.
You cannot get HPV from hugging or holding hands, sharing food or utensils, poor personal hygiene, swimming pools or hot tubs, or toilet seats. You can have HPV even if it has been years since you were sexually active and if you do not have any symptoms.
What are the symptoms of HPV?
Most people will never know that they have HPV. Most HPV types have no symptoms and most people will not develop health problems because of HPV. For most people, their immune system will attack the virus and clear the HPV infection within two years. This is true of both low- and high-risk HPV types. Sometimes the body does not clear the HPV infection.
The low-risk HPV type infections can cause warts on hands, feet, arms and chest, and genital warts. Warts can be treated. Warts caused by low-risk HPV types rarely turn into cancer. About 75% of the HPV types cause warts. The other 25% of HPV types infect the moist surface layers like inside the nose, mouth, throat and eyelids.
The high-risk HPV type infections usually have no symptoms, but this type of HPV can cause cells to change over many years. The changed cells may become cancer.
There is no treatment for the HPV virus itself. Warts and pre-cancer cells can be treated. Cancer in the head, neck, cervical, anal and genital areas can be treated too. It is easier to treat cancer when found early when it is small and has not spread.
HPV-Related Cancer Prevention
Why does HPV increase cancer risk?
HPV and co-infections are very common. About 80 million Americans are currently infected with HPV and about 14 million people will get a new HPV infection every year according to the Centers for Disease Control and Prevention (CDC). HPV infections clear up most of the time without causing problems. If an HPV infection does not clear up and stays in the body, it may cause cancer later in life.
“More than half of all sexually active people contract one or more types of this virus at one time, making it the most common sexually transmitted disease in the U.S. In fact, oral, head and neck cancers associated with HPV are on pace to overtake the incidence of cervical cancer by the year 2020,” according to the Head and Neck Cancer Alliance (HNCA).
Can HPV related cancers be prevented?
Yes! The American Dental Association (ADA), National Cancer Institute (NCI) at the National Institutes of Health (NIH), Centers for Disease Control and Prevention (CDC), American Academy of Pediatrics (AAP), American Cancer Society (ACS) and many other agencies and organizations recommend that children and adults ages 9 to 26 be vaccinated for HPV. People ages 27 to 45 may also receive the HPV vaccines if considered to be at high risk for HPV infections. Talk with a dentist or doctor about being vaccinated for HPV prevention.
The HPV vaccine is safe and very effective in preventing 9 of the 150 known HPV types. The vaccine is called Gardasil®9, and is designed to protect against HPV types 6, 11, 16, 19, 31, 33, 45, 52 and 58 that may cause cervical, vulvar, vaginal, anal, penile, and head and neck cancers.
Facts About the HPV Vaccine
- The vaccine prevents certain cancers that start in the throat, cervix, vulva, vagina, penis and anus. The HPV vaccine works well providing almost 100% protection against infections and pre-cancers caused by certain types of HPV. It is estimated that 90% of HPV cancers can be prevented if with vaccination.
- The HPV vaccine works best when given to children between the ages of 9 to 12. Vaccines are used to help stop diseases by giving children the protection before being exposed to the virus. In the United States (US), most people are exposed to HPV in the teens and early twenties so vaccinating before the age of 12 is best. The body produces the most antibodies to HPV when given before the age of 12. People ages 13 to 26 who did not receive all of the doses or have not been vaccinated should get the vaccine as soon as possible.
- The HPV vaccine is for girls and boys. The vaccine is recommend for all children to help protect them from infection that can cause cancer when they get older. HPV is so common that at least 8 out of 10 people in the US will be exposed to it in their lives. Most HPV infections go away without causing health problems, but we do not know if infections will not go away and may eventually cause cancer.
- The vaccine is safe. The HPV vaccine has been used since 2006. All vaccines including the HPV vaccine have to go through extensive safety testing before they can be used. More than 120 million doses have been given in the US. The vaccine is closely monitored by scientists and health organizations for safety. There are common side effects from the HPV vaccine that go away quickly, like fever or headache. A small number of people may have an allergic reaction to the vaccine. Anyone with a severe allergy to yeast or any other ingredient in the vaccine should not receive the vaccine.
- The vaccine does not contain harmful ingredients. The ingredients in the vaccine help make it effective and safe. All ingredients can be found in the environment, human body and foods. The HPV vaccine contains aluminum like other vaccines. Aluminum boosts the body’s immune response to the vaccine. Every day People are exposed to aluminum in food, cooking utensils, water and even breast milk.
- The HPV vaccine can protect fertility, not harm it. More than 100 studies have shown that the vaccine is safe with no data to suggest that the vaccine will affect your chances of having children later in life. In fact, the vaccine helps protect women from future problems linked to pre-cancer and cervical cancer. The vaccine is a safe way to help protect health and the ability to have healthy children in the future.
- The vaccine lasts a long time. Current research shows that the protection provided by the HPV vaccine does not lessen with time. Research will continue to watch how long protection against HPV lasts. If research shows that vaccine protection does lessen with time, booster shots will be provided.
Who should receive the HPV vaccine?
| Who Should get the HPV Vaccine | # of Doses | When the Vaccine Should Be Given |
|---|---|---|
Children aged 11-12 years, who do not have health conditions that make it difficult to fight infections (can be started in children aged 9-14 years) |
2 |
Second dose: 6-12 months after the first |
Teens and adults ages 15-26 who have not been vaccinated Also, children or adults ages 9-26 years with lowered immunity, talk to your doctor about medical problems that fit this category. |
3 |
Second dose: 1-2 months after the first Third dose: 6 months after the second |
Adults 27 up to age 45 years of age who are at a high risk for HPV with shared clinical decision making |
3 |
Second dose: 1-2 months after the first Third dose: 6 months after the second |
Where to get vaccinations for children and adults
Ask your dentist or doctor about the vaccine for HPV.
- Children can receive the vaccine from their pediatrician, primary care doctor or the county health department. In most cases, the HPV vaccine can be given at the same time as other shots needed for back-to-school.
- Children who are eligible can receive free vaccines before their 19th birthday through the Vaccines for Children program
- Information for Parents regarding Vaccines for Children
For more information on this and other immunizations, visit Missouri Immunization Coalition.
The Merck Patient Assistance Program can be reached by calling 800-727-5400. You may also visit https://www.merkhelps.com/GARDASIL%209
HPV Educational Resources
- American Cancer Society (ACS)
- American Dental Association (ADA) MouthHealthy.org
- Centers for Disease Control and Prevention (CDC)
- Head & Neck Cancer Alliance (HNCA)
- HPV Awareness and Education – HPVANDME, A Non-Profit Organization
- HPV Cancer Resources