What is Antibiotic Resistance
 Overuse of antibiotics is creating stronger germs. Some bacteria are already "resistant" to common antibiotics. When bacteria become resistant to antibiotics, it is often harder and more expensive to treat the infection. Losing the ability to treat serious bacterial infections is a major threat to public health.
Overuse of antibiotics is creating stronger germs. Some bacteria are already "resistant" to common antibiotics. When bacteria become resistant to antibiotics, it is often harder and more expensive to treat the infection. Losing the ability to treat serious bacterial infections is a major threat to public health.
Antibiotics are designed to fight bacteria by targeting specific parts of the bacteria’s structure or cellular machinery. However, over time, bacteria can defeat antibiotics in the following ways:
Survival of the Fittest (Natural Selection)
When bacteria are initially exposed to an antibiotic, those most susceptible to the antibiotic will die quickly, leaving any surviving bacteria to pass on their resistant features to succeeding generations.
Biological Mutations
Since bacteria are extremely numerous, random mutation of bacterial DNA generates a wide variety of genetic changes. Through mutation and selection, bacteria can develop defense mechanisms against antibiotics. For example, some bacteria have developed biochemical “pumps” that can remove an antibiotic before it reaches its target, while others have evolved to produce enzymes to inactivate the antibiotic.
DNA Exchange
Bacteria readily swap bits of DNA among both related and unrelated species. Thus, antibiotic-resistant genes from one type of bacteria may be incorporated into other bacteria. As a result, using any one antibiotic to treat a bacterial infection may result in other kinds of bacteria developing resistance to that specific antibiotic, as well as to other types of antibiotics.
Rapid Reproduction
Bacteria reproduce rapidly, sometimes in as little as 20 minutes. Therefore, it does not take long for the antibiotic-resistant bacteria to comprise a large proportion of a bacterial population.
Antibiotic-Resistant Bacteria and Effectiveness of Those Drugs
To date, all antibiotics have over time lost effectiveness against their targeted bacteria. The earliest antibiotics were developed in the 1940s.
These "miracle drugs" held at bay such devastating diseases as pneumonia and tuberculosis, which had previously been untreatable. But the steady evolution of resistant bacteria has resulted in a situation in which, for some illnesses, doctors now have only one or two drugs “of last resort” to use against infections by superbugs resistant to all other drugs. For example:
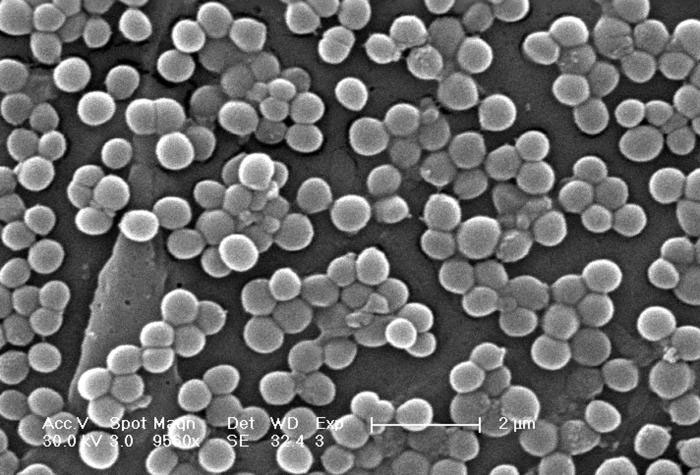
Staph Aureus
Nearly all strains of Staphylococcus aureus in the United States are resistant to penicillin, and many are resistant to newer methicillin-related drugs. Since 1997, strains of S. aureus have been reported to have a decreased susceptibility to vancomycin, which has been the last remaining uniformly effective treatment.
Campylobacter Infections
Today, one out of six cases of Campylobacter infections, the most common cause of food borne illness, is resistant to fluoroquinolones (the drug of choice for treating food-borne illness). As recently as ten years ago, such resistance was negligible.
Next Steps
Clearly, it is important to extend the useful lifetime of any drug that is effective against human disease. And today, this is even more important because few new antibiotics are being developed, and those that are developed tend to be extremely expensive.
Historical Timeline of Antibiotics
- Louis Pasteur unknowingly described the first antibiotic in 1877 when he observed that certain bacteria release substances that kill other bacteria
- In 1909, Paul Ehrlich discovered arsphenamine (Salvarsan), an arsenic compound that kills Treponema palladium, the bacterium causing the sexually transmitted disease, syphilis.
- In 1928 Alexander Fleming discovered that a mold inhibited the growth of staphylococcal bacteria and named the substance it produced "penicillin" (possibly Pasteur's unknown substance).
- It was not until 1940 that Howard Florey and Ernst Chain isolated the active ingredient in Fleming's mold.
- With wide-scale production of penicillin, the use of antibiotics increased, leading to an average eight-year increase in human life span between 1944 and 1972. Unfortunately, many bacterial species continued to survive penicillin treatment due to their resistance mechanisms.
